Ureteropelvic junction obstruction in children by polar vessels: histological examination result
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 15 May 2023
Authors
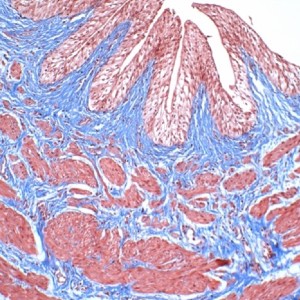
In children, ureteropelvic junction obstruction (UPJO) is mostly caused by intrinsic factors (IUPJO) such as abnormal amounts of muscle and collagen deposition; extrinsic UPJO are rare and often due to crossing vessels (CVs). What is not clear is whether there is also intrinsic UPJ pathology in patients with CV. The aim of our study was to compare the histology of the two types of obstruction and to determine whether these histologic features are distinguishable enough to enable to identify the cause of obstruction based on histologic appearance alone. We retrospectively reviewed pathology reports of 38 children with UPJO that underwent surgery in our hospital from 2008 to 2022. The intrinsic and extrinsic groups consisted of 18 and 20 patients, respectively. After ematoxylin-eosin and Gomori's trichrome staining the specimens were scored for fibrosis and muscular hypertrophy in histhopatology, and CD117 antibody were used to detect interstitial Cajal-like cells. In our study, histological analyses revealed no differences between the CV and IUPJO specimens in terms of presence and degree of fibrosis and muscular hypertrophy; likewise, for presence of interstitial Cajal-like cells.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.