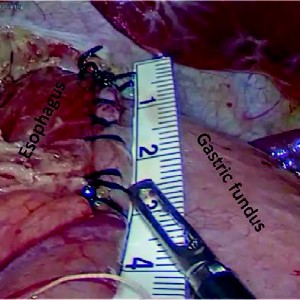
GERD surgery in non-neurologic patients: Modified Laparoscopic Hill-Snow Repair is a valid alternative to Nissen fundoplication. Results of a 20 years of follow-up
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
Nowadays laparoscopic Nissen fundoplication represents the gold standard in surgical treatment of complicated Gastro-Esophageal-Reflux Disease (GERD), above all in cerebral palsy patients. In non-neurological patients without gastrostomy Nissen fundoplication can create some problems (gas bloat syndrome, dysphagia). Laparoscopic Hill-Snow repair is an established surgical alternative, but it is reported only in adult population. We describe our modification of Hill-Snow technique and our experience in a large series of non-neurological children in order to report its effectiveness and applicability in pediatric patients affected by complicated GERD. Between 2000 and 2022, 319 children underwent surgical correction of gastro-esophageal reflux at our Department. All were affected by complicated gastro-esophageal reflux unresponsive to PPI (Proton Pump Inhibitors). 251 underwent laparoscopic Nissen fundoplication; 68 non-neurological patients underwent laparoscopic Hill-Snow repair. Of these 68 children 48 were males (71%) and 20 females (29%); median age was 5years (3 months-11 years). Weight range was 4-37kg.
52 patients (76.5%) presented the following symptoms: retrosternal pain, dysphagia, regurgitation, coughing, failure to thrive, persisting reflux esophagitis. 16 (23.5%) had chronic respiratory problems (aspiration, apneic-spells, dysphagia, coughing, choking, gagging). For 8 (11.8%) symptoms were expression of chronic recurrent gastric volvulus. All underwent modified-laparoscopic-Hill-Snow repair. Contrast study showed sliding hiatal hernia in 55 patients (81%), while endoscopy demonstrated 16 cases of histologically severe esophagitis (23.5%) and 52 of mild esophagitis (76.5%). No intraoperative/postoperative complications were recorded. 60patients had a complete follow-up (range 1-20 years). 60/68 patients were evaluated with barium-swallow-study at 6-12 months; 40/68 patients with upper-gastrointestinal-endoscopy at 12months. No relapse was reported. 50 patients (73.7%) were symptom-free. 18 (26.3%) referred occasional epigastric pain, associated with vomit in 2 cases. 64 (94.1%) referred ability to vomit; 4 temporary difficulty to swallow (average 30 days). All patients reported being able to burp. 3(4.5%) presented episodes of gas-air-bloat during the first 2 months with spontaneous resolution. No case of dumping syndrome was recorded. This technique’s modification yields excellent results in term of relapse and side effects at long-term follow-up. We reported the first and largest pediatric series in non-neurological children with encouraging results.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.